As you may remember from my initial post, My Journey Begins, my journey started with a meeting with Dr Ewing when she confirmed I did have breast cancer. My second post, Breast Cancer Facts & Self Exam, shared how to conduct your own at home breast screening, which I hope you will remember to do at least once a month. I also shared symptoms to be aware of that may be related to breast cancer.

My Journey Continues
After further testing, I had another in-person appointment with Dr. Ewing and her team to share the process moving forward and what their approach is to treating breast cancer. I was also assigned a Breast Cancer treatment team, each with a different specialty.
My UCSF cancer team includes 3 oncologists:
- Dr. Ewing, the Surgical Oncologist
- Dr. Jo Chien, the Medical Oncologist
- Dr. Prionas, the Radiation Oncologist
My Care Team
A surgical oncologist is a general surgeon with speciality training in procedures for diagnosing, staging (determining the stage of cancer) and removal of cancerous growths.
A medical oncologist has specialized training in diagnosing and treating cancer with chemotherapy, hormonal therapy, and targeted therapy. The medical oncologist is the primary care provider for someone diagnosed with cancer. Medical oncologists help patients better understand their cancer diagnosis, such as stage, size of tumor and type.
The final member of the team is the radiation oncologist. The role of the radiation oncologist is to oversee the care of a cancer patient undergoing radiation treatment. The radiation oncologist works with a team that plans the best type and length of radiation treatment. More to come on this when I am in the radiation treatment stage.
I also met with the Medical Coordinator for the I-SPY2 platform trial. This is a trial that has been going on for over 10 years with more than 25 participating hospitals across the country. Some of the new tests scheduled relate to screening for the trial, which tests for the likelihood of recurrence and is used to find the optimal medical therapies. To learn more about UCSF’s I-SPY2 trial click here.
UCSF Overall Treatment Approach:
Dr. Ewing reviewed the overall approach UCSF follows to arrive at the appropriate treatment plan. Once the testing is done, they ask patients to enter Phase 1 of the I-SPY2 trial to assess what “medical” treatment would work best PRIOR TO surgery. Like me, you may be interested to know that this is not a “blind trial” like most of those we see on TV, but a trial to determine the medical protocol most likely to be successful in reducing the size of the tumor.
Dr. Ewing noted that EVERY PATIENT has surgery despite the apparent success of the neoadjuvant medical treatments. They use the term “neoadjuvant” which means “prior to surgery”. They’ve learned that using medical therapies, like chemotherapy and radiation, BEFORE surgery increases the chances of saving the greatest amount of breast tissue.
It may sound strange not to do surgery first. In my case, I was ready to say, “please take them both” (meaning take both my breasts now), thinking that was the best and safest approach to minimizing the spread or recurrence of the cancer.
But, the “neoadjuvant” approach is done because the #1 goal is to “prevent metastasis” or the spread of the cancer cells, and there is always a likelihood of residual cancer cells that need to be removed.
Further Testing:
After my meeting with Dr. Ewing, I was immediately scheduled for additional tests the same afternoon. The goal of these additional tests is to create the best treatment plan given my particular breast cancer. The tests included:
- Another biopsy beyond the FNA (Fine Needle Aspiration”). This “core” biopsy will expand the specimen so they can better assess the type and grade of the cancer cells and their likelihood of responding to a particular drug regimen. Click here to learn more about FNA.
- They will also do an FNA biopsy of the sentinel lymph nodes. The sentinel node is defined as the lymph node to which the cancer cells are most likely to spread from the primary tumor. For more on sentinel lymph nodes, click here.
- They will also complete a “Mammaprint”. The MammaPrint is a test that helps show whether the breast cancer is likely to metastasize (spread to other organs). This test is also used for screening for the upcoming I-SPY2 platform trial. To learn more about a mammaprint, click here .
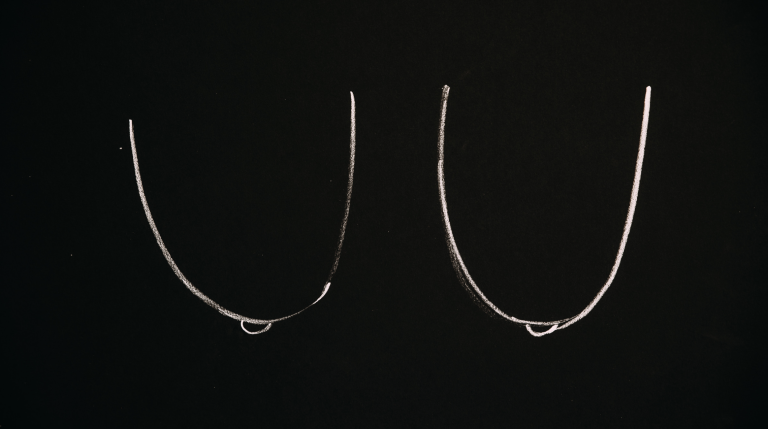
- The final test of the day was another mammogram that is used for mapping and tracking the tumor. This is where they put in trackers to identify and track the breast tissue and lymph node locations and migration. The best way to track the tumor and lymph node is to place a small “clip” in each. The clip is about the size of a grain of rice and is easily seen via ultrasound or other imaging. This clip is then monitored through mammograms to see changes (reduction) of the tumor size.
Thank you for following along on my journey. My goal is to continue to spread education and awareness of breast cancer. The process is daunting and overwhelming as so much information and medical terminology is being thrown at you. It helped me to write it down and then later review it and process it.
If you haven’t already, click the link below to join me so you don’t miss anything along the way.
In next week’s post, I’ll share the results of the testing and the next steps from there.