In my last post, I discussed a few of the surgical options that are common in breast cancer treatment and the differences between a lumpectomy and mastectomy. As previously mentioned, surgery was always a part of my treatment plan and a key milestone for me. This post will discuss my surgical journey and why I chose to have a bi-lateral mastectomy.
MRI Results
As I mentioned in my last post, I had a breast MRI prior to surgery. I met with Dr Ewing, my surgical oncologist, to review the MRI results and images, and unfortunately, my right breast still showed active cancer cells. She shared that she could not be certain of how much there was and how effective a lumpectomy would be. This was the primary factor for why I chose to have a mastectomy. I did not want to have a lumpectomy and then later require another surgery if the team was unable to fully remove all of the concerning and impacted area.
After further discussion and learning more about the procedure, I also decided to do a Bi-Lateral or Double Mastectomy. I felt very blessed and happy to be able to have a choice, especially since I did not have any cancer cells in my left breast, so medically it wasn’t a necessity.
Why I Chose a Bi-Lateral Mastectomy
I chose a double mastectomy for several reasons. Many of the reasons are considered personal choice or cosmetic, rather than medically necessary. I had to continually reminder myself was having a bi-lateral (double) mastectomy vs lumpectomy does not impact the changes of cancer reoccurrence.
The first reason was to make both breasts appear the same. With the medical decision to have a full mastectomy on my right, my left without full tissue removal, would forever look and feel different as a “typical” breast would with age or weight changes. Cancer has forever impacted my body physically and mentally, I wanted to eventually be able to feel confident in my own body. As a single woman who will re-enter the dating the world, I don’t want to feel insecure about what my body will look like. For me, it made sense to have the bi-lateral mastectomy with expander placement. As Dr Ewing stated, even when I am old and saggy, my boobs will still be perky!
Dr. Ewing and I also decided that it would be possible preserve my natural nipples, which is called “nipple-sparing.” This aspect of the procedure is not always feasible for everyone, as the cancer cells can invade the nipple, and in those cases, it is essential to remove them. The goal is to preserve the nipple and needed blood supply, but eliminate all breast tissue. Even in successful surgery the blood supply may not always resume, causing the nipples to die and have to be removed. To learn more about “nipple-sparing” I have included an article from the Massachusetts General Hospital.
Tupperware Ta-Tas
As mentioned in my post, my surgical team included several medical specialists:
- A surgical oncologist, Dr. Ewing
- A plastic surgeon, Dr. Piper, and
- An anesthesiologist.
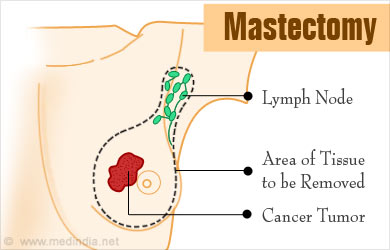
The first step in my surgery was for Dr. Ewing to remove the breast tissue, cancerous tumor(s) and effected lymph node(s). During the second part of the surgery, the plastics team lead by Dr. Piper came in and completed the surgery.
Dr Piper and her team placed tissue expanders, which are similar to temporary implants and I like to call them my “Tupperware Ta-Tas.” The expanders look a bit similar to a breast silicon implant, but are not fully round, the back and bottom are flat. The expanders are used to stretch chest skin and soft tissue before reconstruction. They also prevent pressure from being applied to the skin flaps, allowing blood flow and circulation to the skin so it can recover before the implants are placed. The expanders would later be used to fill and guide my decision to size of intended breasts for reconstruction. Here is a link from Cancer Centers of America to learn more on tissue expanders.
The expanders are particularly important if reconstruction follows radiation. Radiation causes the breast tissue to change shape, or shrink in size, so the expanders will help preserve the skin and tissue so that reconstruction will be easier.
For my treatment plan, I was expected to complete radiation once I healed from surgery. This also meant that my reconstructive surgery could not happen until 6 months after completion of radiation.

Post- Operation
My surgery was initially estimated to take around 4 hours, but the Nurse Practitioner thought that was optimistic and expected it to be more like 5.5-6 hours. In total, I was in surgery for 6 hours. The wait for my parents was agonizing as they were not allowed to wait at the hospital and had to return to their home due to COVID19 protocols.
Surgery was a success as Dr. Ewing was able to remove all the cancerous tissue and gain healthy margins. I only needed to have the sentinel lymph node removed, which was a relief, because as more lymph nodes are removed, there’s a higher risk of lymphedema. I have an included an article about lymphedema from Centers for Disease Control.
I understood that my subsequent rehab would be more complex and challenging since I decided to do a double mastectomy, but I felt in the long run, it was the best decision for me. Following surgery, I had physical therapy to help promote arm movements and healing, as well as to reduce scar tissue. It is very important to do the recommended PT exercises as surgery can reduce or limit arm movements and cause pain.

Conclusion
The Bi-Lateral Surgery would not be the final stop on this journey.
After surgery and healing, I will have radiation, and then hormone therapy for at least the following five years. I will be continually monitored by my team of doctors, with frequent visits, scans and testing.
I am beyond thankful for my amazing team of doctors at the UCSF Medical Center, and feel blessed to have been under their care and treatment. It’s only because of my team and continuous research that I have responded so well to treatment. The more we learn about breast cancer, the better treatment gets.
In my next post I will be discussing the potential side effects of a mastectomy and my personal healing journey post surgery. Thank you all for following along on my journey. I hope you have a very Happy New Year and Happy Holidays! Cheers to 2023!



