In my last post, I discussed the process of using the Delta Dignicap Cold Caps. (I have included a link to take you back to that post if interested.) The goal of using Cold Cap is to freeze the hair follicles, reducing the amount of chemo that impacts those cells, which can reduce the amount of hair loss. The process of using cold cap is time consuming, however, and will typically add time to your chemo treatments.
In this post, I will be talking about my specific chemo regimen and process. Since I was diagnosed with triple positive breast cancer (Estrogen (ER+), progesterone (PR+), and HER2+), the chemo I was given is called TCHP, which is specific to target and kill the cells associated with the Triple+++ diagnosis.
My Chemo Regimen
My chemotherapy (which I’ll often refer to as “chemo”), consists of 4 different medications.
The shorthand for this combination is TCHP, which stands for Taxotere + Carboplatin + Herceptin + Perjeta). I have included a link to learn more about TCHP from Medical News Today, which includes a description of each of the drugs.
- Taxotere and Carboplatin are both classified as chemo drugs.
- Herceptin and Perjeta are hormone-targeted infusion therapies that are not technically “chemo” medications.
This is a very common chemo regimen for breast cancer. In my case, I had 6 chemo infusions, each of which were 3 weeks apart, so it took 4 1/2 months to complete that phase.
Each medication comes with its own side effects and “typical” reaction, but as you’ll see below, you will be given “pre-meds” to help offset some of the side effects:
- Taxotere (T) can cause neuropathy, fluid retention, swelling, nausea and vomiting.
- Caboplatin (C) can cause blood counts to be low and hair loss.
- Herceptin (H) doesn’t have too many side effects, however it can cause cardiac issues, which why I have to have an EKG regularly to monitor my heart function.
- Lastly, Perjeta (P) can cause diarrhea, which typically follows within 7-10 days after the chemo infusion.
The Chemotherapy Process
Before every chemo, I got what are called “pre-meds”, which are medications to minimize any of these side effects. They include anti-nausea meds, Benadryl, a steroid by mouth (to limit the risk of infection), and continuous fluids. I didn’t have to worry about taking any additional medications until the next day since I was already be fully loaded.
A steroid – called dexamethasone – was also prescribed for the night before, the morning of and the night after my chemo infusion. I did have trouble sleeping the night before chemo, but it is hard to say it was solely because of the steroid. I was so exhausted by the time I was home after chemo, I didn’t have any trouble sleeping.
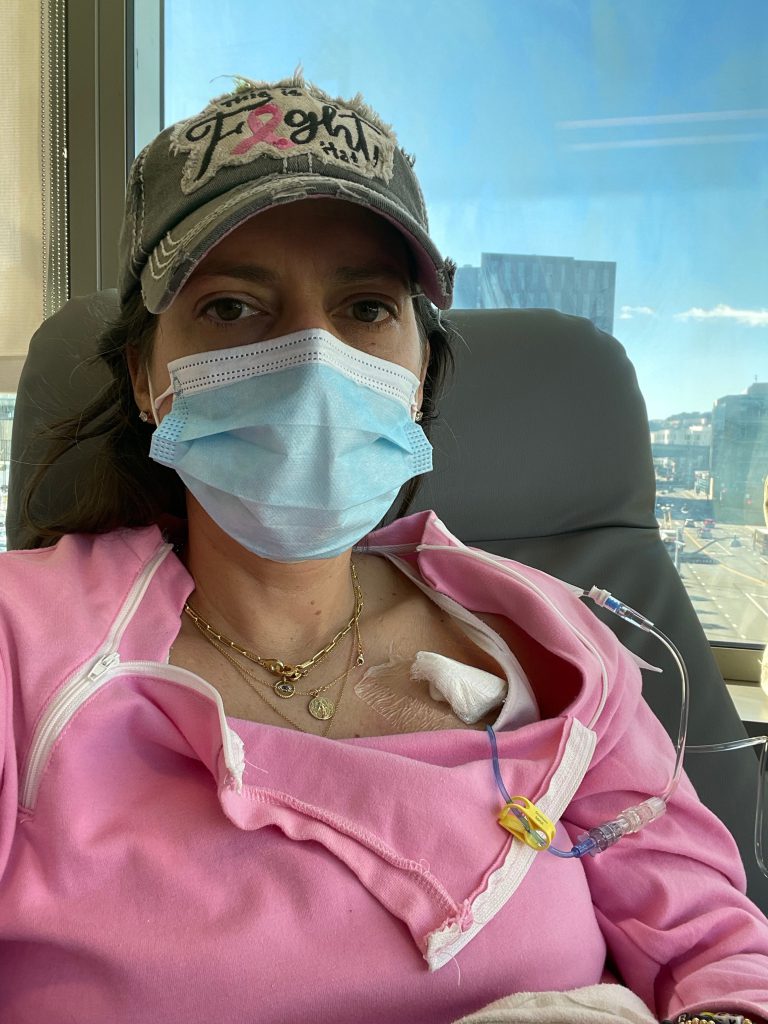
For my initial chemo treatment, I had 2 nurses. Each medication has to be checked and verified with 3 nurses before being administered. The nurses regularly checked on me within every 30-60 minute period to make sure I didn’t have any reactions. The Cold Cap, a procedure I discusseed in a previous post, remained on my head throughout the entire chemo treatment, a total of 8 hours. It made for a VERY long and exhausting day.

Side Effect City
The major side effects I felt were fatigue, weakness and “chemo” brain … meaning I didn’t have much of an attention span or ability to focus or do much. During the 3-4 days after chemo, I struggled a bit more with GI symptoms, nose bleeds, a rash, headaches and more night sweats. My night sweats became even stronger and I would wake up in the middle of the night completely drenched, through my clothes and sheets. I would often get up and change my clothes and sheets.
The good part about the sweating is that it’s the body’s way to show that the chemo is actively fighting the cancer cells. The following days after chemo, my taste buds started to change or go away entirely; nothing really tasted good. I was also very proactive about my oral hygiene as I did not want any mouth sores, so I had to rinse my mouth and brush my teeth after every meal. I would rinse my mouth with baking soda and salt mixture.
Starting the day after chemo, and for about a week following, my appetite decreased and my tongue sometimes felt like old sandpaper. No matter what I would eat it, everything tasted terrible. It seemed like a lot of it was that nothing tasted like what I remembered. That impacted my interest and cravings since I was not excited to eat anything. I found that sticking to more simple dishes such as Ramen, simple soups, noodles, eggs, rice and simple proteins for the first week was best, as I got less frustrated with it all being so bland.

Other Side Effects
My nose, sinuses and lips were also super dry. Aquaphor and the humidifier quickly became my best friends. It is also common during chemo to lose your nose hairs and membranes, along with taste buds.
I had a few strict rules that my oncologist felt were necessary to follow during chemo treatments since I was immunocompromised. I was told not to eat sushi, as raw fish can carry food-borne illnesses.
I was also strongly discouraged from eating in restaurants because this was during the COVID19 pandemic and too risky for me to be around groups of people. Lastly, I was not allowed to go get manicures or pedicures, as I could get an infection from the tools they use.
What I’ve learned about chemo is that it identifies cancer cells because they are fast-moving. Unfortunately, chemo doesn’t yet do a very good job differentiating between “good or bad” cells that move fast. The “normal” cells most commonly affected by chemotherapy because they are fast-moving are the blood cells in the mouth, stomach and bowel, along with the hair follicles which can result in mouth sores, nausea, diarrhea, and/ or hair loss.

Stay In Touch With Your Care Team
I was in continual contact with my care team as we were all tracking my symptoms and reactions. I kept track of any new symptom and how long it lasted. The majority of the symptoms were pretty typical, even 7-10 days after chemo, as some of the medications start to show symptoms at that point.
It typically takes 48-72 hours for chemo to be flushed out of your system, but some medications can still show side effects after that time period. I was very happy to learn from my oncologist that the typical response to chemo will be the same each time, except for fatigue which tends to be cumulative.
The side effects from the first two chemo treatments were the hardest on me, but for the four following treatments were less impactful as it seemed as though my body had, in some ways, adjusted to the regimen. I was also better prepared mentally so I knew what to expect. Fatigue continued to be the main side effect I struggled with.
Family Support
My Mom and Dad shared different roles and responsiblities as they were my primary caregivers throughout my treatments.
After the first chemo treatment, my Mom and Dad split up the duties. My Dad spent every hour of my treatments with me in the hospital while my Mom went to my house to take care of my dogs and prepare a meal I could eat when I got home, which was rarely before 7:00 pm. She also stayed overnight for several days to help and support me as none of us knew what to expect. My Mom is a retired nurse, and she was using her detailed nursing skills daily with me. This was helpful and important for me since I was so out of it for the initial 3-4 days post chemo.
One of the highlights of being in the “cancer club” are the amazing people you will meet along the journey. Sitting in the chemo infusion center chairs for my 6-8 hours of treatment, I met a lot of other cancer warriors and heard many inspiring stories. I will be discussing this more in another post. While it is a club in which you never want to be a member, you also meet some of the best people you will ever meet.
Immune System Booster
Before going home, I was given an Neulasta Onpro patch, which is a small automatic injection device that was placed on my outer arm. The nurse injects the medication into the small device and then places it on my arm. After about 30 seconds I started to hear it tick and then felt a snap, like a strong rubber band snapped against your arm. That snap is the device placing the needle canula into my arm.
The device will then continually flash a small green light and at 27 hours exactly, it will automatically inject the medication into my body. This medication is an immune system booster, helping my body to make WBCs (white blood cells) that fight off infection after cancer treatments. (Medical technology today is AMAZING, isn’t it?)
This drug also comes with some side effects that I felt the last few days, mostly bone pain. For some, the bone pain is almost unbearable. My doctor recommended I take Claritin for 3 days after chemo to help with the discomfort. I’m happy to report that my blood counts remained within normal limits, so overall I’m quite thankful.

Learning to Listen to Your Body
Going through chemo, I learned more how to listen to my body and respond to its needs. Lots of naps, resting and walking at least 30 minutes a day, sometimes making myself get up and walk, and drinking lots of fluids.
One thing that my oncologists shared with me was the importance of walking at least 30 minutes each day, and that getting up and moving around would help to decrease the fatigue. The first two days post chemo, it was almost impossible for me to walk that long. I learned to break it up, even if that meant small 5 minute walks throughout the day. Some days I would just walk in my backyard or throughout the house. Once I was past day 5 following chemo, I was able to walk more and felt more like myself. The days I felt the most “normal” typically were the 3 days prior to the next round of chemo, as my chemo treatments were every 3 weeks. Just in time for the side effects to start all over again.
Conclusion
During this process, I learned that chemo treatments and side effects are very individual. Just as everyone is different, so are the potential side effects you may feel or the intensity of them. I tried not to become too overwhelmed or focused on the insane side effects other people felt, and really wanted to focus on my own journey. I quickly learned to take life one day at a time, and when that was tough, one minute at a time.
Thank you all for continuing to follow my cancer journey. I appreciate the support and love.