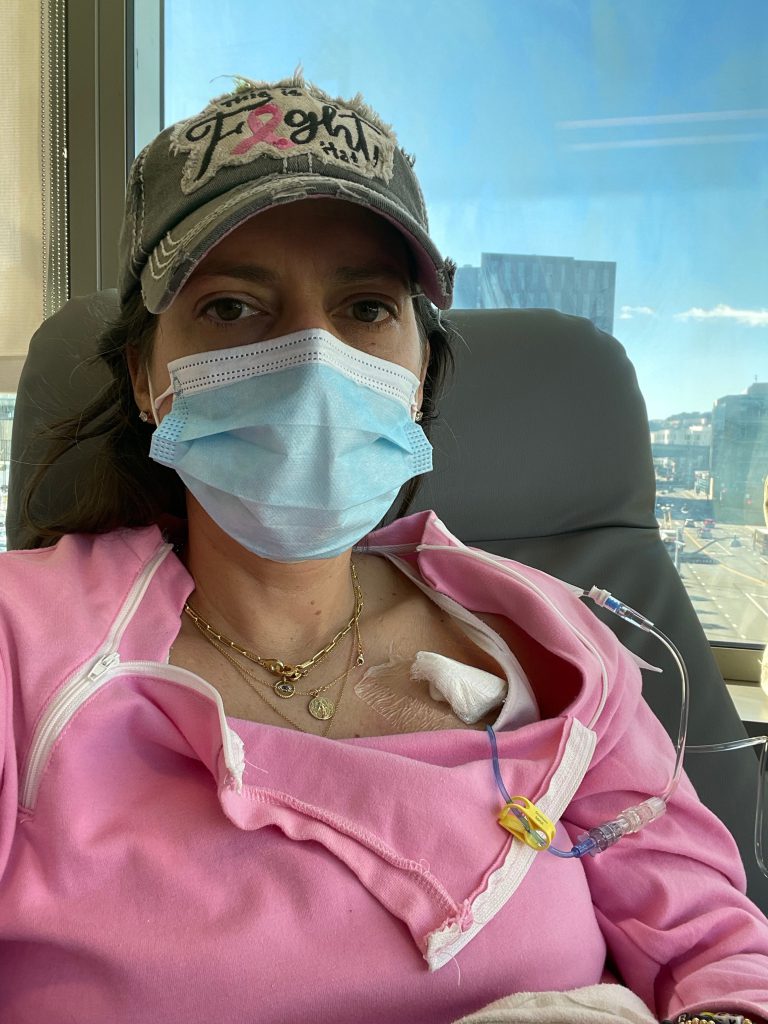
In my last post I discussed having my Catheter Port placed and the reasons for why I chose to have one. The port has a catheter that delivers the chemo straight to my vena cava near the heart, reducing the impact on surface veins. The Port has been a life saver for me and I am very thankful to have it.
The Impact of Chemo on My Tumor
Prior to every chemo treatment, I met with my medical oncologist, Dr. Chien. She would discuss any new side effects I may have been expierencing or any new concerns. She would also measure my tumor prior to each chemo.
The measurements are not exact since it is measured with a tape measure and by physical touch. When I had the initial breast MRI, the size of my tumor was reported as 9.6cm … between the size of a peach and a grapefruit … pretty significant in size and presentation. These measurements are not precise because the density could also be scarring or inflammation rather than the size of the tumor. Nonetheless, the estimates are valuable to measure changes in the size of the tumor over time.
After my 2nd Chemo treatment, Dr Chien measured the tumor and it had shrunk to 6.5 x 7cm from a 9 x 10cm, which is about a 50% reduction, from 90 square centimeters to 45. She thought that was great news and we were certainly heartened by such unexpected progress. The reduction was noticeable to me and comparing the images before starting chemo and after cycle 2, was very exciting and comforting news.

My Tumor Continues to Shrink
Prior to Chemo cycle 4, my tumor had shrunk by 80% after the first three infusions. Dr. Chien also could no longer feel the enlarged lymph nodes in my right arm pit, which was a sign that the chemo had also helped to reduce the tumors impacting my lymph nodes. My breast overall felt more “normal,” less tight and the nipple also started to look more like it used to before the cancer.
For Chemo cycles 4-6 the tumor size was very hard to measure without scans, especially since I have very dense breasts. While Dr. Chien was very happy with my response to chemo, she was uncertain whether I had a full response to chemo without having another breast MRI. A complete response means that there are no longer any active cancer cells in response to treatment. Here is a link to learn more about a complete response to chemo from Breastcancer.org.
Hormone Therapy
Once I completed the 6 cycles of the TCHP chemo regimen, Dr. Chien recommended that I start hormone infusion therapy for one year with the drugs Herceptin and Perjeta; here is a link to learn more about Herceptin and Perjeta from Breastcancer.org.
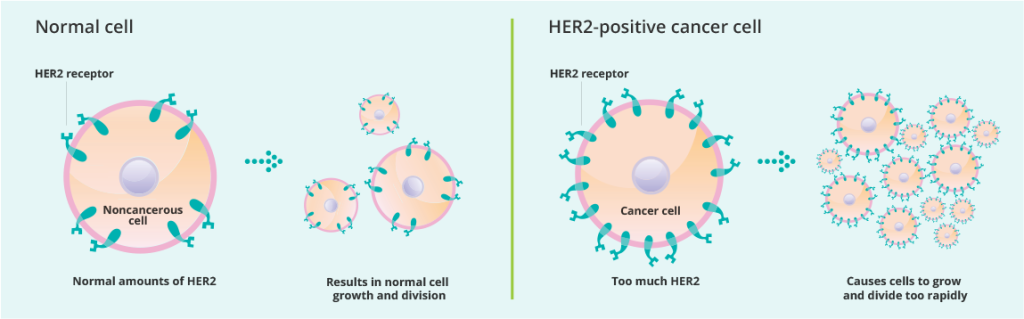
Both Herceptin and Perjeta (H&P) were part of my HTCP chemo infusions, but after the six infusions, I would no longer need the 2 chemo drugs (Carboplatin & Trastuzumab). The infusions were every 3 weeks for 2-3 hours. Herceptin and Perjeta infusions are considered targeted therapy, meaning they are designed to attack specific proteins on certain types of cancer cells like HER2+, that cause them to grow and multiply rapidly. As with the chemo infusions, hormone therapy also comes with a risk because the targeted proteins, like HER+, are also found in normal healthy cells, so the targeted treatments can also affect healthy cells.
Oral Hormone Therapy
After the completion of TCHP, I started oral hormone therapy which will continue for the next 5-7 years. Chemo treatments put me in medically induced menopause, which will continue during the hormone therapy.
The drug I’m on is Letrozole, which is an oral hormone therapy drug used to lower estrogen levels in postmenopausal women; you can learn more about Letrozole here.
I take one Letrozole pill every day for the duration of the treatment. Since my breast cancer diagnosis was Triple Positive, one of which components included estrogen (ER+), it is crucial to maintain lower levels of estrogen in my body to reduce the possibility of the recurrence of my cancer. Since I entered menopause, I have continued to have hot flashes, muscle/joint aches, dryness all over my body, and fatigue.
What’s the Preferred Hormone Drug?
During my surgery, which I will discuss in subsequent posts, the tumor, or what is left of it, was removed and sent to pathology for more specific analysis. The pathology also helped Dr Chien and her team decide what oral hormone drugs were the best option for me. The hormone therapies are designed to manage and keep my hormones within a reasonable range, since I am triple positive for progesterone (PR), estrogen (ER), and HER2.

The Decision to Change the Hormone Therapy
Once the pathology report came back, Dr Chien shared that she wanted me to undergo 14 infusions of Kadcyla instead of Herceptin and Perjeta. I had completed 4 infusions of Herceptin and Perjeta before my surgery and then began Kadcyla infusions after surgery.
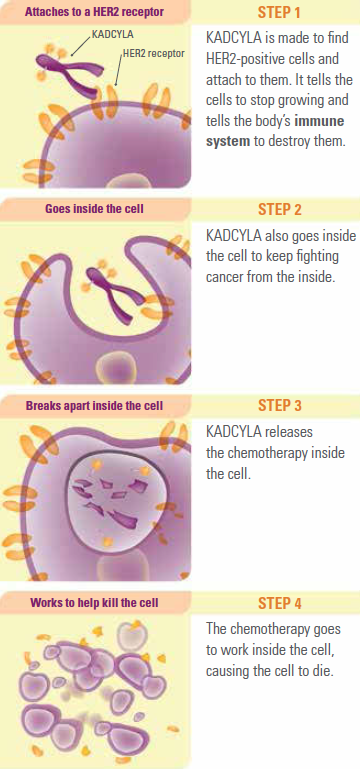
Kadcyla, which is also known as a TDM1, is a combination of chemotherapy and Herceptin, that work together to keep cancer cells from growing. It is used for HER2+ breast cancer (which is what I have) where cancer cells may exist after surgery. The positive aspect is the side effects are more mild than other chemo drugs, but still may include fatigue, neuropathy, bone and joint pain, headaches, bowl issues and nausea. It is important to note, I will not need to wear the cold cap for Kadcyla as hair loss is not a side effect.
I will have 14 cycles of Kadcyla, every 3 weeks in a 30 minute infusion treatment and 30 minute subsequent observation. Kadcyla is believed to bring chemotherapy into the HER2+ cells and kill them. It was designed to cause less harm to normal healthy cells, although it still can affect them. You can learn more about Kadcyla from the Kadcyla patient information page.
In some ways I felt defeated not having a complete response to the previous HTCP chemo regimen and needing to have more chemo. At the same time, I also appreciate having a more aggressive plan of attack to limit recurrence. I think anyone who has gone through cancer carries a fear of a recurrence. It is hard to not think about it and be anxious about what the future might hold, but I hope I will learn how to focus more on the present and trust that the treatment plan will keep me safe.
Conclusion
Thank you all for continuing to join me on my cancer treatment journey. I hope I am providing enough detailed information to be helpful to other breast cancer warriors. In my next blog I plan to share helpful items that I used during chemo treatments. Thank you again.